

These crackle types are defined by the duration of each single crackle. Instead, another subdivision based on crackle characteristics is frequently referred to, namely ‘coarse’ versus ‘fine’. 4 This difference could be explained by the site of airway closure, that is, central airways in obstructive and peripheral airways in restrictive defects.Īlthough Nath and Capel proposed that the timing of crackles could be clinically helpful, which was also supported by Piirilä et al, 1 recent guidelines for diagnosing COPD 5 and heart failure 6 do not mention the distinction between early and late crackles. Few years after Forgacs published his findings, Nath and Capel observed clear differences in the timing of crackles between patients with bronchial obstruction, in whom early crackles usually were heard, and patients with restrictive lung defects, who had late crackles. 2 Since the inflation of the lungs happens sequentially, and the basal parts inflate later during inspiration than the central parts, 3 crackles may be described by time of appearance. 1 Forgacs proposed that crackles heard during inspiration were related to sudden opening of airways. Philadelphia: Lippincott Williams & Wilkins.Crackles are respiratory sounds often heard in chronic obstructive pulmonary disease (COPD) as well as in restrictive conditions, such as heart failure, lung fibrosis and pneumonia. Brunner & Suddarth's Textbook of Medical-Surgical Nursing. Do you have an easy acronym or pearl for remembering breath sounds, or some test-taking strategies to share?īreath Sounds Reference Hinkle, J. Reviewing what you know and thinking about each response choice can help you focus in on the correct answer. During lung auscultation, crackles are heard in pulmonary fibrosis, which is choice B.
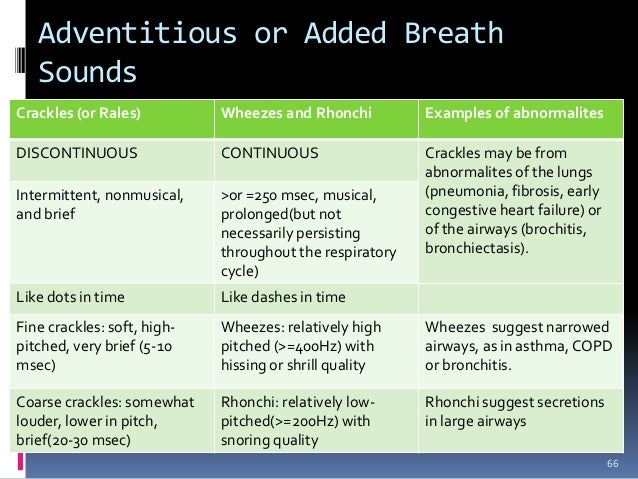
There would be loss of breath sounds over the area of a pneumothorax as there is no air movement in the area of auscultation. In general, there are not specific adventitious breath sounds associated with neuromuscular disorders.Ī pneumothorax is a collapsed lung. Diaphragmatic weakness can lead to hypoventilation chest wall muscle weakness can lead to ineffective cough and upper airway muscle weakness can lead to difficult swallowing and ineffective clearing of upper airway secretions. Neuromuscular disorders can cause respiratory problems through several pathways as the muscles responsible for breathing are affected. The crackles are the result of the snapping open of collapsed, stiff alveoli. This may be hard to distinguish from congestive heart failure. The most common adventitious breath sound associated with pulmonary fibrosis is fine bibasilar crackles. This scarring leads to thickness and stiffness in the lungs. Pulmonary fibrosis is a form of interstitial lung disease in which scarring (or fibrosis) is the hallmark clinical feature. For testing purposes, however, expiratory wheezes are associated with asthma. Initially the wheezes are expiratory but depending on confounding factors or worsening clinical symptoms, there may be inspiratory wheezes, rhonchi or crackles. As air moves through these narrowed airways, the primary lung sound is high-pitched wheeze. This response is triggered by an irritant, allergen, or infection.

The resulting physiologic response in the airways is bronchoconstriction and airway edema. AsthmaĪsthma is a condition mediated by inflammation. In this instance, it would be helpful to go through each clinical condition separately and predict what you may hear on auscultation. Now, let’s think about test-taking strategies.
RALES LUNG SOUNDS CAUSE PROFESSIONAL
Establishing Yourself as a Professional and Developing Leadership Skills.



 0 kommentar(er)
0 kommentar(er)
